Heart attack on a chip: Scientists model conditions of ischemia on a microfluidic device
Researchers led by biomedical engineers at Tufts University invented a microfluidic chip containing cardiac cells that is capable of mimicking hypoxic conditions following a heart attack—specifically when an artery is blocked in the heart and then unblocked after treatment. The chip contains multiplexed arrays of electronic sensors placed outside and inside the cells that can detect the rise and fall of voltage across individual cell membranes, as well as voltage waves moving across the cell layer, which cause the cells to beat in unison in the chip, just as they do in the heart. After reducing levels of oxygen in the fluid within the device, the sensors detect an initial period of tachycardia (accelerated beat rate), followed by a reduction in beat rate and eventually arrhythmia which mimics cardiac arrest.
The research, published in Nano Letters, is a significant advance toward understanding the electrophysiological responses at the cellular level to ischemic heart attacks, and could be applied to future drug development. The paper was selected by the American Chemical Society as Editors' Choice, and is available with open access.
Cardiovascular disease (CVD) remains the leading cause of death worldwide, with most patients suffering from cardiac ischemia—which occurs when an artery supplying blood to the heart is partially or fully blocked. If ischemia occurs over an extended period, the heart tissue is starved of oxygen (a condition called "hypoxia"), and can lead to tissue death, or myocardial infarction. The changes in cardiac cells and tissues induced by hypoxia include changes in voltage potentials across the cell membrane, release of neurotransmitters, shifts in gene expression, altered metabolic functions, and activation or deactivation of ion channels.
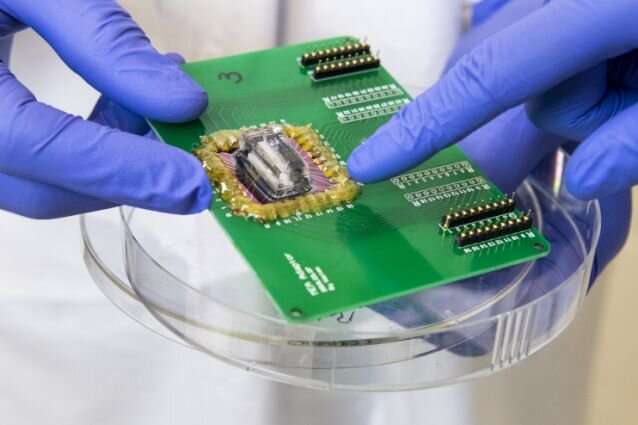
The biosensor technology used in the microfluidic chip combines multi-electrode arrays that can provide extracellular readouts of voltage patterns, with nanopillar probes that enter the membrane to take readouts of voltage levels (action potentials) within each cell. Tiny channels in the chip allow the researchers to continuously and precisely adjust the fluid flowing over the cells, lowering the levels of oxygen to about 1-4 percent to mimic hypoxia or raising oxygen to 21 percent to model normal conditions. The changing conditions are meant to model what happens to cells in the heart when an artery is blocked, and then re-opened by treatment.
"Heart-on-a-chip models are a powerful tool to model diseases, but current tools to study electrophysiology in those systems are somewhat lacking, as they are either difficult to multiplex or eventually cause damage to the cells," said Brian Timko, assistant professor of biomedical engineering at Tufts University School of Engineering, and corresponding author of the study. "Signaling pathways between molecules and ultimately electrophysiology occur rapidly during hypoxia, and our device can capture a lot of this information simultaneously in real time for a large ensemble of cells."
When tested, the extracellular electrode arrays provided a two-dimensional map of voltage waves passing over the layer of cardiac cells, and revealed a predictable wave pattern under normal (21 percent) oxygen levels. In contrast, the researchers observed erratic and slower wave patterns when the oxygen was reduced to 1 percent.
The intracellular nanoprobe sensors provided a remarkably accurate picture of action potentials within each cell. These sensors were arranged as an array of tiny platinum tipped needles upon which the cells rest, like a bed of nails. When stimulated with an electric field, the needles puncture through the cell membrane, where they can begin taking measurements at single cell resolution. Both types of devices were created using photolithography—the technology used to create integrated circuits—which allowed researchers to achieve device arrays with highly reproducible properties.
The extracellular and intracellular sensors together provide information of the eletrophysiological effects of a modeled ischemic attack, including a "time lapse" of cells as they become dysfunctional and then respond to treatment. As such, the microfluidic chip could form the basis of a high throughput platform in drug discovery, identifying therapeutics which help cells and tissues recover normal function more rapidly.
"In the future, we can look beyond the effects of hypoxia and consider other factors contributing to acute heart disease, such as acidosis, nutrient deprivation and waste accumulation, simply by modifying the composition and flow of the medium," said Timko. "We could also incorporate different types of sensors to detect specific molecules expressed in response to stresses."
More information: Haitao Liu et al, Heart-on-a-Chip Model with Integrated Extra- and Intracellular Bioelectronics for Monitoring Cardiac Electrophysiology under Acute Hypoxia, Nano Letters (2020). DOI: 10.1021/acs.nanolett.0c00076
Journal information: Nano Letters
Provided by Tufts University





















